Shining a light on lung cancer
Lung cancer is Australia’s fifth most common cancer, with 13,250 people diagnosed every year.
Throughout November – Lung Cancer Awareness Month – the Lung Foundation Australia worked to shine a light on lung cancer and support research into the development of treatments, diagnosis pathways and one day, a cure.
Lung cancer remains our nation’s leading cause of cancer death. It is therefore crucial we continue to raise public awareness of this devastating disease and support ongoing research all year round.
Improving understanding of the potential risk factors for lung cancer and the signs and symptoms of the disease among the community will help to improve early detection, diagnosis and treatment.
About lung cancer
The two main types of lung cancer affecting Australians are, non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC).
NSCLC
SCLC
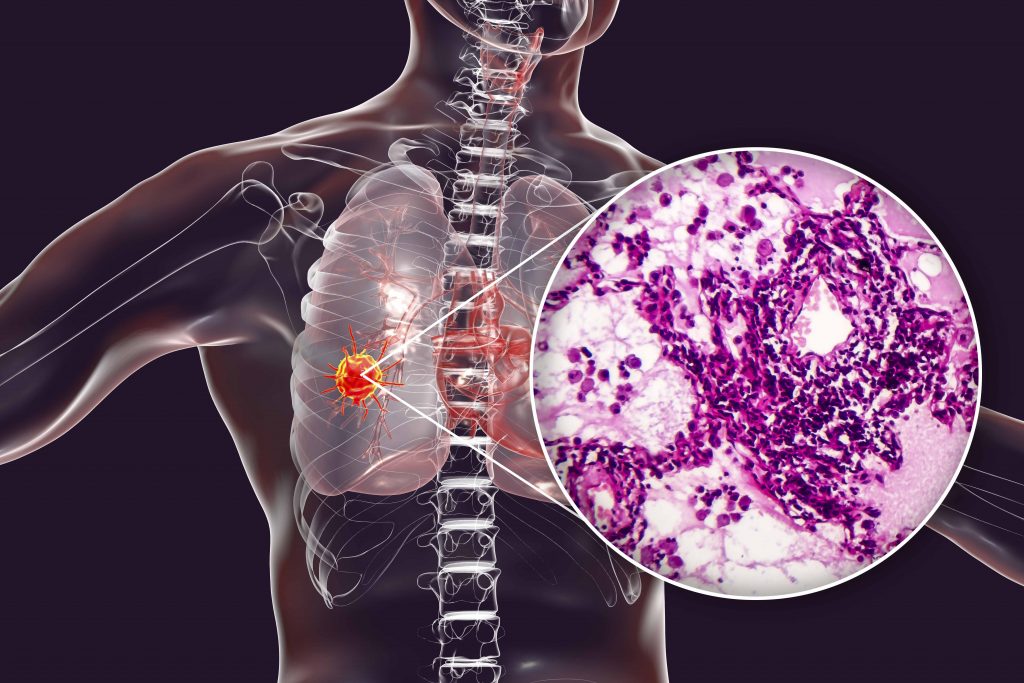
NSCLC accounts for up to 85 per cent of all lung cancers, the most common types of NSCLC are adenocarcinoma, squamous cell carcinoma and large cell carcinoma1. Adenocarcinoma begins in the cells responsible for producing mucus. It is the most common cancer in both smokers and non-smokers. Squamous cell carcinoma commonly develops in the larger airways of the lungs. Large carcinoma can be found in any part of the lung and cannot be clearly identified as either squamous cell or adenocarcinoma.
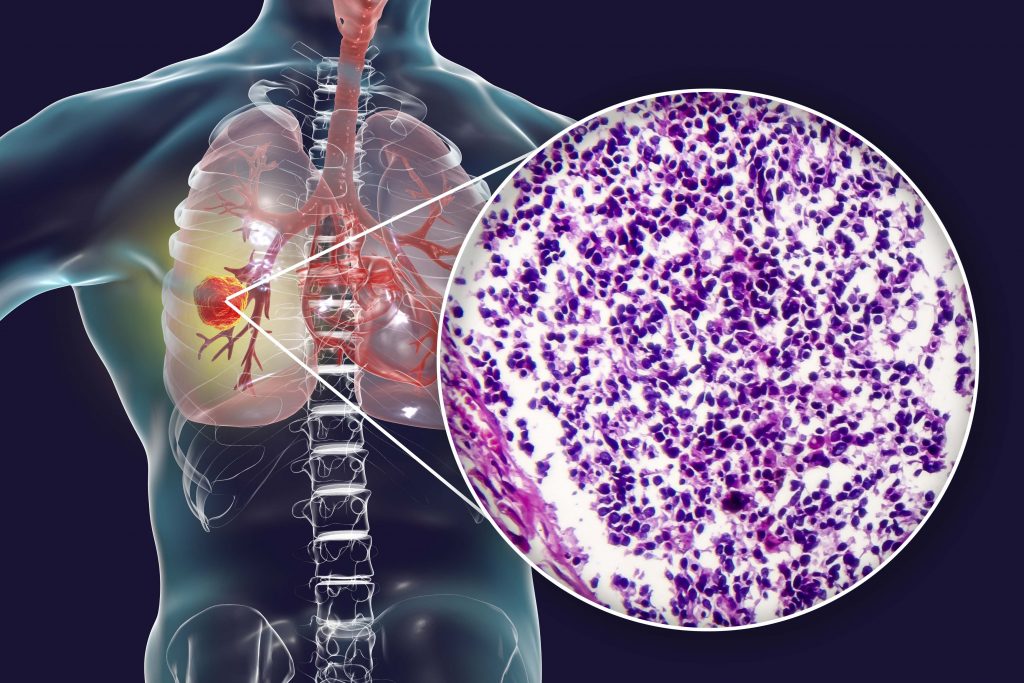
SCLC is an aggressive, highly complex form of lung cancer, characterised by extremely rapid growth and early, widespread metastases. SCLC accounts for 15% of all lung cancer cases2. This form of lung cancer is known as a neuroendocrine tumour, which means it affects the neuroendocrine cells found in the lining of the airways. The aggressive form cancer has one of the lowest survival rates of all cancers, only 17 percent of people diagnosed survive beyond five years.
SCLC is most commonly diagnosed in those over the age of 60 due to lifestyle factors, however, the disease can also affect younger people.
Risk factors
The risk factors for both SCLC and NSCLC are similar however the most common risk factor for developing SCLC is tobacco exposure, including cigarette smoking and second-hand smoke inhalation.
Multiple risk factors can contribute to the onset of the disease, including environmental and genetic factors. Family history of lung cancer increases the risk in both smokers and non-smokers. One-in-five people with lung cancer have never smoked.
Workplace and industrial exposure to cancer-causing agents can also increase one’s risk to lung cancer. These agents include, crystalline silica, chrysotile asbestos, arsenic, beryllium or nickel.
Symptoms
The stigma around lung cancer, along with the devastating symptoms and poor survival rates, can significantly affect the psychological wellbeing and social lives of both those living with the disease and their families. Individuals who were previously smokers and are diagnosed with lung cancer can be left feeling ashamed.
The importance of early diagnosis
Early detection of lung cancer can prevent or delay lung cancer progression. Currently, up to 50 per cent of NSCLC and more than 70 per cent of SCLC have already progressed to stage IV by the time of diagnosis. Detection at this advanced stage makes them incredibly difficult to treat and lowers the chance of survival.
It is therefore crucial to help improve awareness of the early symptoms and the importance of speaking to your doctor if you think you may be at risk.
VIVA! has proudly partnered with the Lung Foundation Australia and industry on several occasions to highlight the significant toll lung cancer can take on those affected and their families, and sharing the stories of real Australians diagnosed with the disease.
Importantly, through this work, we also helped to address the stigma associated with lung cancer and raise awareness of the latest advances in treatment.
For more information on lung cancer and how you can support ongoing research, head to https://lungfoundation.com.au/
- National Cancer Institute. Non-small cell lung cancer treatment – Health professional version. Aug 2019]; Available from: https://www.cancer.gov/types/lung/hp/non-small-cell-lung-treatment-pdq#_4.
- Cancer Australia. Types of lung cancer. Aug 2019]; Available from: https://lung-cancer.canceraustralia.gov.au/types.
